Imagine yourself on a roller coaster ride, with unexpected twists and turns at every corner. Now, envision this roller coaster as a metaphor for the perplexing journey of a condition known as multiple sclerosis (MS). It is a fascinating odyssey that delves into the intricate workings of the human brain and challenges our understanding of the enigmatic realm of neurology.
Multiple sclerosis, commonly referred to as MS, is a chronic autoimmune disease that primarily affects the central nervous system, specifically the brain and spinal cord. Its name, derived from the Latin words "multiple" and "sclerosis" meaning "many scars," reflects the characteristic feature of this condition: the development of scar-like lesions within the nervous system. These lesions disrupt the transmission of electrical impulses, giving rise to a wide array of symptoms. While more prevalent in temperate regions, MS has been observed across the globe, defying geographical patterns. According to the National Multiple Sclerosis Society, approximately 2.8 million people worldwide are affected by MS, with about 300 people receiving a diagnosis every day. This highlights MS’s significance as a global health concern.
Similar to an illusionist conjuring an array of tricks, MS presents itself through a variety of symptoms, making diagnosis a formidable puzzle for physicians. In MS, the immune system mistakenly targets the brain and spinal cord, resulting in damage to the protective coatings of nerves. This interference disrupts the efficient transmission of messages between the body and brain, leading to various challenges in communication. Common signs include fatigue, numbness or tingling sensations, muscle weakness, difficulty with coordination and balance, and impaired vision. These symptoms can vary greatly between individuals and may come and go, mimicking a magician's vanishing act. To further complicate matters, MS has several distinct subtypes. The most common form is relapsing-remitting MS (RRMS), characterized by periods of relapse with symptom flare-ups, followed by periods of remission where symptoms partially or completely disappear. Other subtypes include primary progressive MS, secondary progressive MS, and progressive relapsing MS, each displaying unique progression patterns and challenges. Notably, in RRMS, the incidence in women is nearly three times higher than in men, with an average onset age of 30. However, in primary progressive MS, there is no significant difference in incidence between genders, and the average age of onset is around 40[1].
Although the exact cause of MS remains elusive, it is believed to stem from a complex interplay of genetic and environmental factors. Genetic predisposition, viral infections, low levels of vitamin D, and smoking have all been implicated in the development of this puzzling condition. Evidence suggests that MS is an autoimmune disease characterized by the immune system's attack on myelin tissue, which is a fatty substance that surrounds and protects nerve fibers in the central nervous system[2]. Yet, the puzzle pieces of MS etiology are still being assembled, leaving researchers eager to unravel its intricate origins.
The management of MS aims to slow disease progression, alleviate symptoms, and improve the quality of life for those affected. A range of treatment options is available, allowing healthcare professionals to tailor therapeutic strategies to each individual. Currently, medicinal therapies targeting MS exhibit various mechanistic effects, including immune cell depletion, growth suppression, and migration inhibition. As a result, they effectively regulate or decrease inflammatory processes occurring in the peripheral immune system, blood-brain barrier, or central nervous system, facilitating MS management[3].
During the acute phase of MS treatment, the primary focus is on alleviating exacerbation symptoms, shortening disease duration, and preventing complications. Glucocorticoids are the primary medication employed for this purpose. In the remission phase, disease-modifying therapies (DMTs) serve as the fundamental pillar of MS management. Available in various forms, these medications aim to reduce the frequency and severity of relapses, delay disability progression, and prevent new lesions from forming. Additionally, symptomatic treatments, including physical and occupational therapy, assistive devices, and medications targeting specific symptoms, offer relief and support in managing the challenges posed by MS.
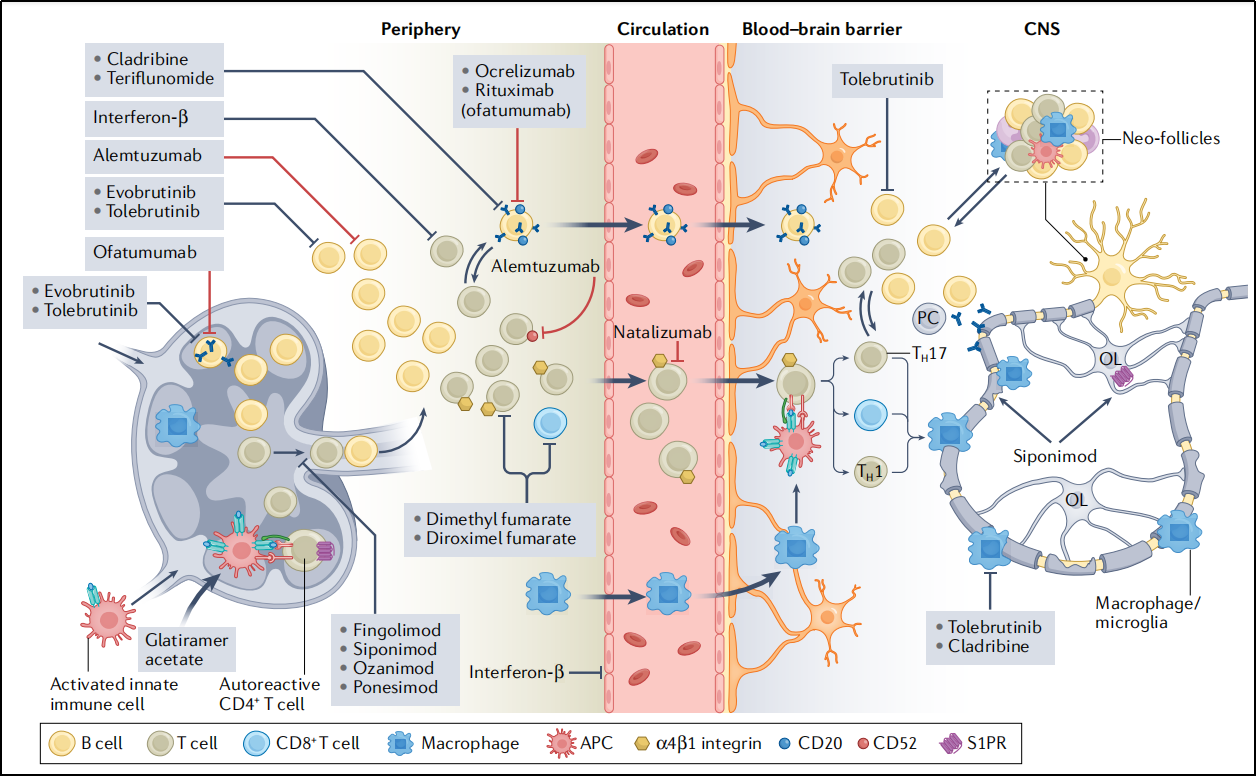
Targets of Current Disease-Modifying Therapies in MS[3]
As scientists tirelessly strive to uncover more effective treatments for MS, the development of novel drug therapies relies heavily on the application of disease models. One such model is Experimental Autoimmune Encephalomyelitis (EAE), which has proven invaluable in advancing our understanding of this complex autoimmune disease. EAE is characterized by specific sensitized CD4+ T-cell-mediated responses, focal infiltration of mononuclear cells around small blood vessels within the central nervous system, and demyelination of nerve fibers. It mimics several phenotypes observed in human MS and is widely recognized as an ideal animal model for studying this enigmatic condition.
GemPharmatech, a dedicated research institution, has successfully developed the EAE model for preclinical evaluation of drug efficacy. By utilizing this model, researchers can gain insights into the underlying mechanisms of MS and test potential therapeutic interventions in a controlled experimental setting. This invaluable tool facilitates the identification and evaluation of promising drug candidates, bringing us closer to finding new avenues of treatment for individuals living with MS.
Reference:
1. Stephen L. Hauser, Bruce A.C. Cree.Treatment of Multiple Sclerosis: A Review[J].Am J Med.2020 Dec;133(12):1380-1390.
2. Tafti D, Ehsan M, Xixis KL. Multiple Sclerosis. [Updated 2022 Sep 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan.
3. Bierhansl L, Hartung HP, Aktas O, Ruck T, Roden M, Meuth SG. Thinking outside the box: non-canonical targets in multiple sclerosis. Nat Rev Drug Discov. 2022;21(8):578-600.


